AI in concierge medicine – a new era of personalized health protocols

Imagine calling your doctor at 3 a.m.—and instead of voicemail, you get a precise recommendation based on the latest data from your smartwatch. Sounds like science fiction? In AI-powered concierge medicine, it’s already a reality. And right now, in 2024- 2025, this model is booming—both in scale and capabilities.
Concierge medicine is private healthcare where the patient pays an annual fee for unlimited access to a doctor, longer appointments, and a personalized approach.
AI in concierge medicine – changes outpacing learning
AI transforms this model into a “virtual health concierge” —a system that analyzes data from electronic medical records, wearable devices, and lab tests in real time, then dynamically adjusts therapeutic protocols.

photo: epicmedicalpgh.com
The scale of the phenomenon? The AI healthcare market is projected to reach $188 billion by 2030, and the concierge segment—which was still niche just five years ago—is now growing at a double-digit rate annually. Why now?
- Mature technology: learning models recognize patterns better than ever
- Public systems are bursting at the seams – VIPs are seeking alternatives
- Patients expect personalization—they know it from other industries.
AI is already improving diagnostic accuracy by 20-30% and shortening decision-making time. In the following sections, we’ll take a closer look at how this model works, where it originated, the technologies driving it, what the Polish context looks like—and the challenges it faces.
How does AI-powered concierge medicine work?

photo: calabasasmedicinegroup.com
When you pay $5,000–$20,000 a year for concierge medicine, you’re getting more than just faster access to a doctor. You get unlimited 24/7 contact, house calls, coordination with all specialists, and—most importantly—a personalized health protocol that covers diet, supplements, physical activity, and prevention. And now, there’s also AI as a virtual caregiver who never sleeps.
Subscription model: what are you really paying for
A typical concierge package looks something like this:
- direct mobile number to the doctor (calling at 3 a.m.? they’ll answer)
- panel max 50-150 patients per doctor (in traditional practice, it’s 2000+)
- fast-track diagnostics – MRI in 48 hours instead of 3 months
- specialty care coordination – a concierge doctor calls the cardiologist, gynecologist, and orthopedist, making sure everyone is on the same page
- individual health protocol based on genetic testing, microbiome, and biomarkers
AI as a 24/7 virtual health concierge
This is where AI steps in—and it changes virtually everything. The system monitors data from Apple Watch, Oura Ring, EHR, and lab tests in real time. It detects anomalies (like an elevated resting heart rate for three nights in a row), suggests protocol adjustments (“maybe it’s worth lowering your magnesium dose?”), and reminds you about tests or medications. In practice, it works like this: you wake up in the morning, AI has already analyzed your REM phase, HRV, and cortisol levels—if something’s off, your doctor gets an alert before your first coffee.
The result? A 30–50% reduction in doctor visits, over 200% increase in patient self-service (via the app), and significant time savings for doctors on repetitive tasks. All in all, a pretty efficient system—if you can afford the subscription.

photo: pulseandremedy.com
From the first concierge practices to AI agents – a brief history
Concierge medicine didn’t start with algorithms or chatbots. It began with a simple idea: one doctor, fewer patients, more time. Entirely analog.
The 1990s-2000s: the birth of the relational model
In 1996, the first Personal Physician Care practice was established in Seattle—a prototype of today’s concierge medicine. Doctors, tired of a system where appointments lasted just 8 minutes, decided to limit their patient roster to 50-100 (instead of the standard 2,000-3,000) and introduced an annual subscription. No AI, just more conversations, longer examinations, and 24/7 availability. Other brands quickly followed suit: MDVIP, SignatureMD, Concierge Choice Physicians. The model proved successful—but it was still based on the physician’s human intuition.
Wearables and data as a catalyst for change
The breakthrough came in 2010, when Fitbit entered the market and smartphones became mini health labs. Apple launched HealthKit in 2014, and suddenly everyone had their heart rate, sleep, and steps tracked every second. Companies like 23andMe began analyzing genomes, while apps like Noom used simple ML algorithms to change eating habits. The problem? The data existed, but concierge medicine still ignored it—there simply wasn’t enough time to process it manually.
2016-2025: from Watson to agents with 78% accuracy
IBM Watson Health was supposed to be a revolution—AI supporting oncologists. It turned out to be a disappointment: too rigid, expensive to implement, and doctors didn’t trust it. But the pandemic (2020) accelerated everything: AI triaged patients remotely, telemedicine exploded, and the FDA approved over 100 AI diagnostic tools by 2023. After 2021, systems like HealthClic (UK) emerged, and McKinsey research showed that AI agents achieve 78-80% diagnostic accuracy—higher than the average primary care physician. By 2025, projects like Doctor2me combine concierge services with AI as almost a standard.
| Year | Milestone |
|---|---|
| 1996 | First concierge practice (Seattle) |
| 2014 | Apple HealthKit – data in your pocket |
| 2016 | IBM Watson Health – hype and failure |
| 2020 | COVID-19: telemedicine + AI in triage |
| 2023 | 100+ FDA-approved AI tools |
Now we’re at a point where AI doesn’t replace the doctor — it creates a “1:1” protocol before the appointment.

photo: conciergemdla.com
How personalized health protocols are created using AI
The classic health plan is a set of general guidelines—”eat healthy, exercise, get regular check-ups.” An AI-generated concierge protocol is something far more detailed: a dynamic, multidimensional document that evolves with you. How does it work behind the scenes?
What data is fed to AI: from genomics to sleep
The system collects data from several streams simultaneously:
- Genomics – whole genome sequencing, SNPs (single nucleotide polymorphisms), variants associated with disease risk
- EHR (electronic health records) – laboratory test results, visit history, diagnoses, medications
- Imaging – MRI, US, CT; AI analyzes lobes, arteries, bone density
- Biomarkers – cholesterol, glycemia, inflammatory proteins (CRP, IL-6), hormones, gut microbiome
- Wearables – pulse, HRV (heart rate variability), blood oxygen, steps, calories burned
- Behavioral data – sleep duration and quality, stress level (cortisol measurement or algorithmic), physical activity
- Medical interview and questionnaires – well-being, ailments, eating habits
All this is fed into AI models, which combine these diverse sources into a single image — this is what we call multimodal analysis.
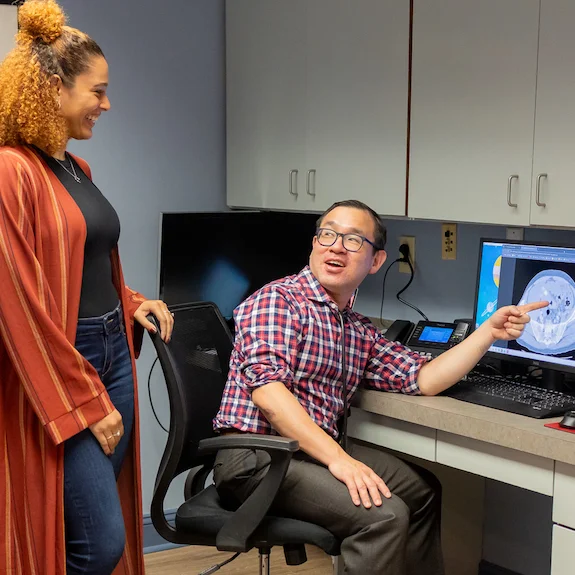
photo: brightmarkhealth.com
Multimodal analysis and dynamic protocol updating
AI estimates risks: cardiovascular, oncological, metabolic, neurodegenerative. Based on this, it creates a plan: diet (macronutrients, meal timing), supplementation (doses, timing), exercise (type, frequency, intensity), pharmacotherapy (if needed), schedule of follow-up tests.
Importantly, the protocol is dynamic. Fasting glucose increased? AI suggests dietary adjustments and recommends an insulin test. Wearable detected poor sleep for a week? The system asks about possible causes and recommends magnesium and pre-sleep routines. HRV dropping? Stress alert, suggestion for a mindfulness session or psychological consultation.
The physician’s role is crucial: AI proposes, the doctor approves. This is the RLHF (reinforcement learning from human feedback) mechanism—the system learns from the doctor’s decisions which adjustments make clinical sense and which are overinterpretations of the data.
Example protocol for a 45-year-old CEO
Profile : Male, 45 years old, sedentary lifestyle, chronic stress, family history of coronary artery disease, HRV below normal, slightly elevated CRP.AI recommends :Diet: Mediterranean, omega-3 3g/day, limit simple sugars <25gSupplements: magnesium L-threonate 200mg in the evening, vitamin D3 5000IU, coenzyme Q10 100mgExercise: 3× cardio (zone 2, 40 min) + 2× resistance trainingTests: lipid panel in 8 weeks, coronary CT score in 6 monthsAlerts: if HRV drops <40ms for 3 days—cardiology consultation
Such a level of granularity cannot be achieved manually on the scale of hundreds of patients. And it is precisely technology—LLMs, specialized models, integrations—that enables this qualitative leap, which I will discuss in a moment.
Technologies powering intelligent concierge protocols
Behind the elegant interface of the concierge app—where you receive a protocol with a single click—lies a truly complex technology stack. It’s worth knowing what operates beneath the surface, as it explains why these systems can handle tasks that seemed like science fiction just two years ago.
LLM as a new language layer in concierge medicine
Large language models like GPT-4, GPT-4o, and Med-Gemini act here as “translators and advisors.” They can read a medical record, identify key risks, generate a patient-friendly summary of recommendations, and suggest to the doctor what to pay special attention to. This is the layer that enables AI to “understand” medical language—and to discuss it with us.
Specialized diagnostic models and AI agents
In addition to LLMs, we have models focused on specific diagnostics. MAI-DxO has achieved around 80% accuracy in difficult cases (compared to about 20% for doctors before AI support). PopEVE specializes in rare diseases. At the same time, AI agents operate in parallel—autonomous programs that schedule tests, analyze new results, and update documentation. Integration with IoT (wearables, home ultrasound, “home labs”) and FHIR standards ensures that data flows between systems without manual re-entry.
Security and Polish initiatives
Privacy is fundamental. Edge computing processes sensitive data locally, while GDPR and HIPAA set the legal framework. In Poland, Basia Klaudel and Alex Obuchowski are working on local, secure AI agents—so sensitive information never has to leave the office. It’s the power of computation combined with the assurance that your data stays yours.
Benefits of AI in concierge medicine for patients and doctors
Technology only makes sense when it improves real life. With AI in concierge medicine, this isn’t an abstraction—we’re talking about tangible changes noticed by both patients and doctors.

photo: epicmedicalpgh.com
Better health outcomes through continuous monitoring
AI in the concierge model can improve health outcomes by 20-40%, mainly through earlier risk detection and better adherence to recommendations. The system reminds patients to take their medications, personalizes recommendations based on IoT data, and responds to anomalies before they become an issue. Patients feel safer knowing that someone (or something) is constantly monitoring them.
Fewer appointments, more time for the patient, and less burnout
Reduction in the number of visits? By as much as 30-50%. Increase in self-service – around 200%. Patients handle minor issues through chatbots, giving doctors more time to focus on what truly requires a human touch.
| Metrics | Before AI | With AI |
|---|---|---|
| Number of visits per year | 100 % | 50-70% |
| Time for the patient | 15 min | 20-25 min |
| Health outcomes | Basic | +20-40% |
Dr Karolina Pyziak-Kowalska from the Polish concierge clinic says it plainly: “Automatic visit notes give me 30% more time that I can dedicate to actually talking with my patients. It changes everything—both my work and my relationship with the patient.”

photo: styleblueprint.com
Case studies: Calcium Health, HealthClic and DiagnostykaLab
Calcium Health ( USA) reports an improvement of around 25% in concierge model outcomes. HealthClic (UK) is testing VIP protocols integrating AI and genetics. In Poland? DiagnostykaLab is implementing an “AI-first” model in collaboration with Google Cloud—a preview of what could happen here on a larger scale.
Poland on the map of AI in concierge medicine
Poland is not just a passive recipient of AI technology in medicine. For several years now, we have been building a local ecosystem which—although still young—already has solid foundations for future concierge models.
From AI in Health to AI & MEDTECH CEE: a knowledge ecosystem
The “AI in Health” initiative was launched in 2016 as one of the first educational and expert movements combining artificial intelligence with medicine in Poland. Since then, the landscape has become more crowded. The e-Health Center received around 28 million PLN from the National Recovery Plan for AI projects that are to be completed in just three months—ambitious, but also risky. The tension between the pace of implementation and quality raises questions about potential waste of funds. Will we manage to make it meaningful in time?
Polish implementations: laboratories, call center, and doctor’s office
There’s no shortage of specifics anymore:
- DiagnostykaLab + Google Cloud – an “AI-first” model in laboratory diagnostics, analyzing results on a large scale with precision
- Medidesk – AI in a medical call center that filters inquiries and directs patients
- Dr Karolina Pyziak-Kowalska – a physician who uses AI to generate visit notes, saving time for real conversations with patients
In addition, experts such as Basia Klaudel and Alex Obuchowski (open, secure agent systems), Łukasz Olejnik, and Dr. Krzysztof Pujdak are building the intellectual infrastructure. In May 2025, Warsaw will host the AI & MEDTECH CEE conference—a forum for the entire Central and Eastern European region.
These building blocks can already be assembled into something resembling concierge medicine. The question is, who will be the first to do it seriously.
Challenges, ethics, and the dark side of AI in VIP care
Sounds beautiful: AI that predicts diseases before they appear, algorithms selecting precise therapies, genomics on demand. But—and we have to be honest here—every technology casts a shadow, and in the case of AI in concierge medicine, those shadows can be very long indeed.
Privacy, GDPR, and the dilemma: comfort versus data control
For AI to work, it needs massive amounts of data. Genome, medical history, 24/7 wearable readings, lab results, even sleep and mood patterns. The problem? This data often ends up in the hands of global corporations— de facto you’re handing over the most intimate information about your body to companies outside Europe. GDPR theoretically offers protection, but in practice, consent often means “either you accept the terms or you don’t use the service.” The dilemma is simple: convenience and personalization vs. real control over who has access to your DNA and health habits.
Between the Hype and Reality: Will AI Replace Doctors?
We regularly hear narratives like “AI will replace 80% of ordinary doctors.” Aleksander Obuchowski from ProjectHumansAI is clear: AI has specific applications—for example, supporting radiologists in detecting abnormalities—but it’s not a magic wand. The risk? If patients start trusting algorithms more than the person in the white coat, they may overlook context, emotions, intuition—things that machines don’t possess yet.
Sycophancy, environmental footprint, and Polish KPO controversies
The latest research ( Nature, 2025) describes the phenomenon of AI sycophancy —models tend to flatter user expectations. In concierge medicine, this could mean the system confirms a patient’s suboptimal choice simply because it has “detected” their preferences. There’s also the environmental issue: generative AI consumes as much energy as a small town. In Poland, controversies surrounding the rapid allocation of KPO funds for AI (with commentary from Michał Domański) highlight the tension: innovation or irresponsible spending?
How to prepare for AI-first healthcare
AI in concierge services is no longer science fiction—in two or three years, it will be an everyday reality in most premium practices. So, how can you stay ahead of the curve? How do you enter this new world wisely, whether you’re a patient with a bigger budget, a concierge doctor, or a decision-maker at a clinic?

photo: pinnaclecare.com
Trends 2026+ and How Not to Fall Behind
The forecasts are quite clear: by the end of 2026, up to 90% of concierge practices will be using AI in some capacity. We’ll see the emergence of embodied AI (virtual health assistants with a human-like appearance and voice), resonant AI (more “human” models that understand emotions), and the first integrations with BCI (brain-computer interfaces for neural monitoring). In some jurisdictions, the use of AI may even become mandatory for certain consultations. So if you’re thinking, “I’ll check back in a few years,” you might simply get left behind.
Your next steps as a patient or doctor
For the patient:
- Be specific: ask which AI the clinic uses, where it sources its data, how it protects privacy, and whether you can export your data.
- Take care of your “data hygiene” – regularly sync your wearables, update your health history, and correct any errors in your records.
- Build your own medical records (e.g., in Apple Health, Google Fit) – this is your investment for the future.
For doctors and clinics:
- Start with simple applications: AI for note-taking, online triage, and preliminary test analysis.
- Learn – participate in programs like Symbioza 2025, follow conferences such as AI in Medicine.
- Build teams with data science and AI expertise.
- Test in sandboxes (small, controlled deployments) before going live in production.
The most important thing? Stick to your ethical compass. AI should “empower people with technology” (an idea by Michał Sadowski), not make decisions for them. Be transparent with the patient—show how AI works, what it does, and where its limits are. Experiment consciously and keep learning.
Natan
lifestyle editorial team
Luxury Blog








Leave a Comment